GYNAECOLOGY
Commitment to women’s well-being
She also has appointments to Macquarie University Hospital and Sydney Adventist Hospital.
Dr Yang’s specialties and interest in the management of

Abnormal cervical screening test (CST) result
The Cervical Screening Test is a simple procedure to check the health of your cervix. If you have ever had a Pap test, the way the test is done will feel the same.
The five-yearly Cervical Screening Test replaced the two-yearly Pap test. If you're aged 25 to 74 you should have your first Cervical Screening Test two years after your last Pap test.
The Cervical Screening Test is more effective than the Pap test at preventing cervical cancers, because it detects human papillomavirus (known as HPV). The Pap test used to look for cell changes in the cervix, whereas the new Cervical Screening Test looks for HPV which can lead to cell changes in the cervix (see diagram of the cervix below).
Once you have had your first Cervical Screening Test, you will only need to have one every five years instead of every two, if your results are normal.
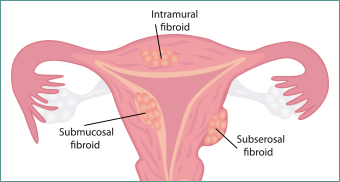
Uterine Fibroids
Fibroids are the most frequently seen tumours of the female reproductive system. Fibroids, also known as uterine myomas, leiomyomas, or fibromas.
Symptoms of uterine fibroids may include:
- Heavy or prolonged menstrual periods, sometimes resulting in anaemia and iron deficiency.
- Abnormal bleeding between menstrual periods
- Pelvic pain (caused as the tumour presses on pelvic organs)
- Frequent urination
- Low back pain
- Pain during intercourse
- A firm mass, often located near the middle of the pelvis, which can be felt by the physician

Heavy Periods
Refers to excessively heavy period bleeding. This can cause iron deficiency in many women, resulting in excessive tiredness, lethargy and poor exercise tolerance. Common causes include Adenomyosis and Fibroids.

Abnormal/Irregular uterine bleeding, Postmenopausal bleeding
Abnormal bleeding means irregular bleeding between normal menstrual periods, or bleeding after menopause.

Uterovaginal Prolapse
Uterine/Vaginal prolapse occurs when pelvic floor muscles and ligaments stretch and weaken and no longer provide enough support for the pelvic floor structures. As a result, the uterus with/without vagina slips down into or protrudes out of the vagina.
Common symptoms include
- Sensation of heaviness or pulling in your pelvis
- Tissue protruding from your vagina
- Urinary problems, such as urine leakage (incontinence) or difficulty passing urine
- Trouble having a bowel movement
- Feeling as if you're sitting on a small ball or as if something is falling out of your vagina
- Sexual concerns, such as a sensation of looseness in the tone of your vaginal tissue
Urinary incontinence
Incontinence is a term that describes any accidental or involuntary loss of urine from the bladder (urinary incontinence) .Common incontinences are Stress incontinence or Urge incontinence. Many patients have symptoms of both stress and urge.

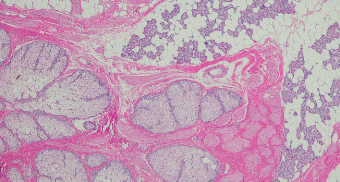
Endometriosis
Endometriosis occurs when the cells lining inside uterus move to other parts of your body. Although they can move to almost any part of the body, most commonly endometriosis occurs in the pelvis.
Endometriosis is very common affecting at least 1 in 10 women.
Common symptoms include
- Painful periods, usually starting 1-2days before the bleeding, often affecting normal activities, causing missing school or work
- Painful intercourse
- Pain when opening bowel especially during a period
- Pain radiating to the back, upper thighs or buttock
- Difficulty in getting pregnant
The treatment of endometriosis often involves both medication (tablets and injections) and surgery (laparoscopy to remove the endometriosis). Most women who have endometriosis will require both of these treatments at different stages of their lives. The choice of treatments depends on how bad the pain is, where the pain is, and if you are trying to get pregnant.
- Medicines:
Pain relief medication (analgesics) like naprosyn or ponstan - Hormone-based treatments
The oral contraceptive pill (‘the pill’) Using an oral contraceptive to stop ovulation, the levels of estrogen in the pelvis are reduced and this can help settle the activity of endometriosis. It is important to realise that use of oral contraceptives will not make endometriosis go away. - Mirena
Mirena is a small device that is shaped like a T. This is placed in the uterus and releases a progesterone-like hormone. This has been shown to reduce the activity and pain of endometriosis over time for many women. - Dienogest (Vissane) is a progesterone treatment that has been shown to reduce the regrowth of endometriosis if it is taken everyday.
- GnRH-agonists
Some implants and sprays can switch off the release of reproductive hormones in women. However, this can induce a state like menopause that women may find unpleasant. It is unusual to use such medications alone for more than a few months, as there can be long-term side effects.
It is important to realise that the medications used for treatment of endometriosis are commonly contraceptive (they stop pregnancy occurring). - Surgery
The surgery depends on the symptoms and the location of the endometriosis. It is usually done by laparoscopy or using a Robot. This procedure allows your surgeon to diagnose and to treat your endometriosis. The endometriosis is cut off (resected ).
Ovarian Cysts
Ovarian cysts are fluid-filled sacs in the ovary. They are common and usually form during ovulation. Ovulation happens when the ovary releases an egg each month. Many women with ovarian cysts don't have symptoms. The cysts are usually harmless.


